Fewer Opioids, More Pay: New Tack on How Doctors Prescribe Them
Some doctors in Michigan are prescribing as few as four opioid pills for pain relief after a common gall bladder surgery.
And, in return, they are paid 35 percent more for doing the surgery in tandem with patient education.
The plan is an effort by Blue Cross Blue Shield of Michigan to reduce the number of opioids prescribed. It works like this:
In pre-operative consultations, participating doctors walk patients through ways to reduce pain without using opioids, like icing and switching between ibuprofen and acetaminophen. When the doctors pull out their prescription pads, they prescribe the bare minimum of pills, ranging from four to 10, depending on the surgery.
That is far fewer pills than are traditionally prescribed. A cholecystectomy—where the gall bladder is removed—is one of the most common surgeries in Michigan. Doctors typically prescribe between 40 to 120 pills for that surgery, according to David Bye, a health-care analyst and project leader for Blue Cross Blue Shield of Michigan.
The plan is a reaction to the opioid epidemic and a tidal wave of drug abuse that’s swallowed up billions of dollars in state and federal funds. But it also adheres to a growing philosophy within health-care circles that reimbursement models should shift to reward quality, not quantity.
The payment plan was designed by the Michigan Opioid Prescribing Engagement Network (OPEN)—a collaborative of insurers, doctors, state government, and the University of Michigan. Blue Cross Blue Shield of Michigan appears to be the only insurer that pays doctors to use this type of pain program. However, other BCBS branches have expressed interest in the payment plan, Bye said, so it has the potential to spread to other states.
Insurers are increasingly weighing in on ways to combat the opioid crisis. For example, Cigna no longer covers the opioid OxyContin (oxycodone), a Purdue Pharma product, for consumers who are insured through their job. Instead the insurer encourages patients to use Collegium Pharmaceutical’s Xtampza ER, an oxycodone equivalent with abuse deterrent properties.
The general reasoning behind BCBS of Michigan’s initiative is if patients are taking fewer opioids, or don’t have access to them unnecessarily, then there will be fewer chances to become addicted. And some patients don’t take all the pills they’re prescribed, so decreasing the number of pills they receive post-surgery decreases the possibility that someone else could get their hands on them.
“They’re interested in incentivizing good patient care,” Chad Brummett, a doctor who helped create BCBS of Michigan’s payment plan, said. “It’s about attentive pain care” versus immediately jumping to opioids to control pain.
The Centers for Disease Control and Prevention declined to comment on this specific program, but said “reducing exposure to prescription opioids, for situations where the risks of opioids outweigh the benefits, is a crucial part of prevention.” The agency has its own prescribing guidelines it published in 2016.
35 Percent More
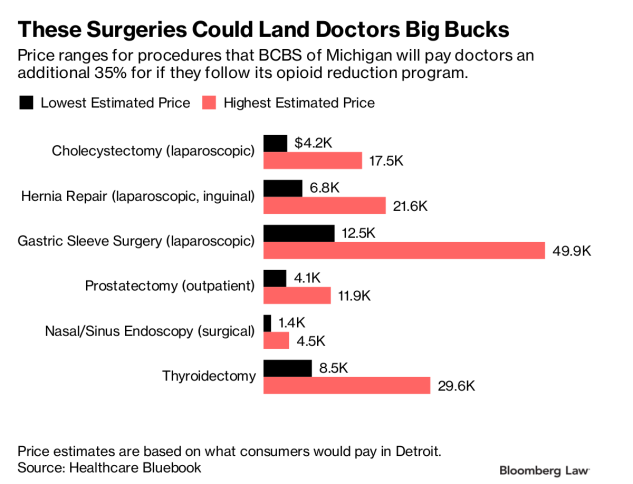
Right now, six procedures are eligible for the payment plan: cholecystectomies, inguinal hernia surgeries, sleeve gastrectomies, prostatectomies, sinus surgeries, and thyroidectomies. These procedures are not particularly invasive or painful, which is why they’re covered in this payment plan.
Cholecystectomies can cost roughly $4,200 to $17,500, according to estimates from Healthcare Bluebook for laparoscopic cholecystectomies in Detroit. Location and insurance coverage impact the price.
With that price range, doctors can make roughly $1,470 to $6,125 more for the same surgery using this payment plan because the 35 percent increase is applied to the total cost of the surgery, not just the physician fee.
Despite the huge payout, BCBS of Michigan isn’t expecting it to hurt their bottom line. In fact, Bye is expecting this to save the insurance company money in the long run.
“Addicted patients are very expensive down the line,” Bye said. Costs add up for anything from addiction treatment, to overdose care, to the litany of health problems that can show up later, “especially with a lot of opioids users turning to heroin as supplies dry up.”
‘Modifier 22′
Doctors who want to participate in the prescription plan are reimbursed at a higher rate when they use a “modifier 22″ in their bill. Modifier 22’s aren’t just used in this context. They’re generally used when surgeries are expected to be more difficult, like surgery on an obese patient, and provide for higher reimbursement levels
Bye said that though he’s not concerned about potential fraud in the program, BCBS of Michigan can audit the program by checking the medical records of doctors, who are supposed to keep a written record of the pre-op pain consultation. The insurer doesn’t require doctors to follow a script or ask specific questions in their pre-operative consultations, but Michigan-OPEN provides some guidance on its website on what doctors should discuss with patients, including whether they’re taking medications like sleep aids.
However, there’s no requirement to address whether a patient suffers from chronic pain in order to receive the higher surgery payout. That presents issues for patients in chronic pain, Jianguo Cheng, president of the American Academy of Pain Medicine, a physician, and a pain specialist, said.
Cheng is also wary of possible conflicts of interest. “If the physician has an incentive to reduce pain medication as much as they can then that could create a problem,” Cheng said.
Word of the payment plan is slowly making its way across the state, and Bye said BCBS of Michigan is already looking into what other surgeries could use this payment system. The insurer has gotten about 80 bills using this payment pathway since the insurer started the reimbursement program in July. It’s open to anyone performing these procedures statewide.
“The data is already starting to show there are lower volumes of pills being prescribed,” Bye said. “So from a plan perspective there is good movement, and it’s good for the physicians across the board.”
Filed under: General Problems



















This is wrong in so many ways. First of all, the surgeon should be in charge of medications and post op care, not the insurance company. Under this policy, the company and the dr basically says, it doesn’t matter if you suffer so I can make extra money! Decisions concerning post op care should be made by two people- the patient and physician. If this isn’t disclosed to the patient, it is wrong. It will do nothing but cause undue suffering.
Yea there plan is working so well to with a increase of drug death of about 10 to 20% including this past year. Prescription drugs have been cut down about 40% but the death keep on happening. This is happening because kids now go to alcohol to heroin pill and usually start snorting it and has there tolerance increase and they need to buy more for there fix they move to injecting it. By the time they get to that point they are spending the entire day from doing whatever to get money to shooting up and then zoning out. Then when they wake up they start all over again.
We have to stop this madness where money is the incentive for corruption. As a people we are slipping further down. I would like to think and hope that we are just about to the bottom so we can start climbing back out. Those of us that follow the rules are right out in the open and under control of those that make the rules. We can fight back by not supoorting these entites and voting govt officials OUT!!!! They are rich and we are the struggling poor.
Stated they educating patients? Who’s educating them or government? Insurance companies state doing it to prevent addicts down the line, we know it’s about bottom line. They still believe and propagate that this is a prescription opioid problem with there heads in the sand of the true causes. What about the chronic pain sufferers? How do they get relief if they’re already on medication but can’t get the same thing while under surgeons care or actually would need more due to additional acute pain which would be so much worse for a cpp. What about treating ppl with a one size fits all dose when everyone metabolizes differently? I believe they just don’t want ppl getting relief for there pain because then they have to pay for the medication monthly! If they’re trying to save cost in the long run with a person needing rehab and taking heroin and overdoses and killing themselves then what’s the problem, as long as they are dead or buying illegal heroin then they’re off the hook for paying but if a person says they have chronic pain and the doc treats them long term for instance so they can continue to work, etc. Then insurance winds up paying. If person can’t get meds then can’t work or stay on insurance so they get away with not paying again. They don’t want these kinds of clients. Just the ones who pay every month and never have problems. Lol, in a perfect world. Wouldn’t we all love to be those ppl, probably used to be but back to reality I’m a chronic pain sufferer and will not have needed surgery because of non or inadequate pain relief!
It seems like this practice should be required to me disclosed to the patient. The patient can then realize that a doctor has an incentive to leave them in increased pain for the doctors own monetary gain. This action in itself becomes part of the medical procedure.
I wonder if there is a way to notify all of the so affected patients in this area in order that they can ask the doctor if they are on the incentive program to collect money for leaving these patients exposed to increased acute pain and also the potential to develop a chronic pain situation.
This explains a lot. Fairly recently I had my left ovary and tube removed, as well as endometrial lesions removed. Zero pain meds. My insurance carrier was BCBS and the doctor said they wouldn’t approve them for surgery.
So how much more suffering has to take place before people recognize and accept the REAL cause of addiction? See the video The REAL cause of drug abuse on http://www.doctorsofcourage.org/videos/.
I gotta confess I get tired of the ads for DOC…I call ’em “ads” b/c when you go there, you gotta buy a membership to read anything. Just what we need….more shills.
Good God almighty. Every time I think the opioid hysterics & money grubbers have gone as low as possible, they plumb new depths. Any doctor who chooses sadistic torture & monetary gain over patient welfare ought to lose their frigging license.
The percentage of patients who become addicted following surgery is less than 1% (https://www.bmj.com/content/360/bmj.j5790). You can positively inflate someone with opioids after surgery for the week or 10 days they’re usually needed and get NO increased risk of addiction. The ONLY thing that happens when you refuse to treat acute pain adequately is to hugely increase the likelihood of the patient developing chronic pain (see same reference above).
The people who become addicted following surgery generally already have addiction issues; these people, unless they get locked in a bubble (or a cell), will always be in danger of getting addicted to something. Happily subjecting 99+% of patients to monstrous suffering will do nothing to change that, & nothing to change the so-called “epidemic,” since it’s not due to Rx meds anyway & is not even an epidemic.
I sincerely, devoutly hope that every doctor who grabs the cash & goes for sadism, & every person behind this policy, suffers the tortures of the damned of unrelieved pain for the rest of their lives. When in God’s name is this nationally approved & applauded hysteria of sadism going to finally hit a turning point?
You got that right. Incentivizing doctors to not prescribe reasonable pain medication – and a week or two weeks worth after a surgery, pending a re evaluation by the doctor is reasonable- is just inhumane.
There’s stories surfacing how celebs and rich people still get pain meds… Like we all knew would happen. It’s the average Joe citizen who is getting tortured with all these draconian, arbitrary rules. Addicts still have no problem getting the illegal shit, it just costs more.