The maker of the EpiPen is being sued under a law that’s typically used to take on organized crime
http://www.businessinsider.com/mylan-class-action-lawsuit-over-epipen-2017-4
Christina Kollmeyer’s son has a allergy that requires him to carry an EpiPen, the emergency auto-injecting devices available that can be used to treat severe allergic reactions.
When Kollmeyer, who has a high-deductible health plan, picked up her son’s prescription in January, she paid $735.09 for two two-packs of the devices.
That’s up from the $313.38 she paid for the same amount in October 2016.
Now, Kollmeyer is one of three women taking the fight to the company that makes the EpiPen: Mylan.
Kollmeyer, along with Amber Rainey and Lisa Vogel, filed a class-action lawsuit on Monday in Tacoma, Washington that claims EpiPen-maker Mylan engaged in a scheme with pharmacy benefit managers, or PBMs — companies that act as intermediaries between pharmacies, insurers and drug companies — to dominate the market and overcharge consumers.
“As a result of Defendant’s scheme, Ms. Kollmeyer overpaid for EpiPens,” the complaint said. The women involved in the suit paid anywhere from $53.94 to $453.49 for two-packs of the EpiPen and EpiPen Jr.
This isn’t the first time a citizen has filed a lawsuit over the price of the EpiPen. In September, an Ohio woman filed a case against Mylan claiming the price increases violated Ohio’s consumer protection law.
Monday’s, however, is the first to focus on the role of PBMs and to bring claims under the Racketeer Influenced and Corrupt Organizations Act, a federal law historically used against organized crime.
Mylan spokeswoman Nina Devlin declined to comment.
Mylan was called out in August 2016 for raising the price of the EpiPento $608.61 from $93.88 over the past decade. It caught the nation’s attention because parents were refilling their kids’ prescriptions, and some found that they were on the hook for hundreds of dollars for the device. The company now sells a $300 generic version.
The plaintiffs in Monday’s lawsuit say Mylan paid large rebates to PBMs so they would favor EpiPen over competitors. In helping Mylan control 95 percent of the epinephrine auto-injector market, the rebates artificially inflated EpiPen’s sticker price, resulting in higher costs for many patients, the suit said.
The lawsuit says the three largest U.S. pharmacy benefits managers – CVS Caremark, part of CVS Health; Express Scripts Holding Co and OptumRX, part of UnitedHealth Group Inc – aided Mylan’s alleged scheme. PBMs may later be added as defendants on the lawsuit, The Wall Street Journal reports.
Pharmacy benefit managers are the companies responsible for negotiating rebates to the prices drugmakers set, and are meant to favor the most effective drug. This is meant to help keep prices low. Many question how effective they are at doing that, however and some have said they could be part of the reasonwhy prices are skyrocketing.
The plaintiffs are seeking damages to represent a nationwide class of EpiPen purchasers.
Filed under: General Problems



















I hope this company gets slammed . Not letting people get these epi pens caused deaths . How do you ever pay for that.losing their money is the only way to make these companies stop. That’s all they care about is money not people’s lives. They need to lose their license.
In reality, the PBM’s ( CVS Health, Express Scripts, Optimum ) are the real “bad guys”.. they are demanding rebates/kickbacks from the Pharmas up to 50% of the price.. in order to keep the Pharma’s product on the PBM’s formulary. With the PBM’s paying for some 90% of all prescriptions and the majority of that 90% controlled by the three that I mentioned. IMO… we have too many for profit middlemen involved in the delivery of healthcare… The entities that are directly providing services (hospitals, prescribers, pharmacies) are the ones that are getting the “financial crumbs” from the healthcare table. All of these middlemen inserted themselves into our healthcare system under the premise that they were going to be able to make the system function more efficiently and save the system money. Now that they have control of 90% of the prescription market place… those of us who understand “the system” see that their primary focus is to increase their market share and increase THEIR PROFITS… Their actions – step therapy, quantity limits, prior authorizations and limiting what meds they will pay for… clearly demonstrates that they have little concern about the pt’s quality of life.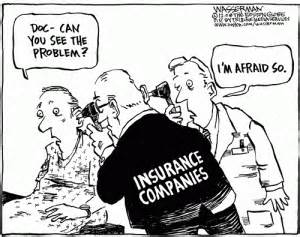
I hope the women don’t get a judge who’s been bought and paid for by PBMs or the drug companies. It’s ludicrous to think that there’s a valid reason for the huge price increases especially when it’s a drug that has been on the market for as long as Epi-pen!