Wedgewood Pharmacy Survey Demonstrates Negative Impact of Opioid Shortages on Veterinarians, Pet Owners, and Pets
http://www.thecourierexpress.com/business/wedgewood-pharmacy-survey-demonstrates-negative-impact-of-opioid-shortages-on/article_69b24b26-1e39-5a80-9168-dc25cad11fa5.html
SWEDESBORO, N.J.–(BUSINESS WIRE)–Sep 14, 2018–A nationwide survey shows that there are unintended consequences for veterinary medicine caused by the Drug Enforcement Administration’s (DEA) efforts to address the national opioid crisis. Opioids in animal medicine are the foundation, and often the only method, of pain control and anesthesia. They are critical for the treatment of animals that have been hit by a car, shot by a gun, mauled by another animal, undergone surgery, or suffer from a severe disease or other trauma. Most pet owners, regulators, elected officials, and state board of pharmacy members are not aware of the repercussions.
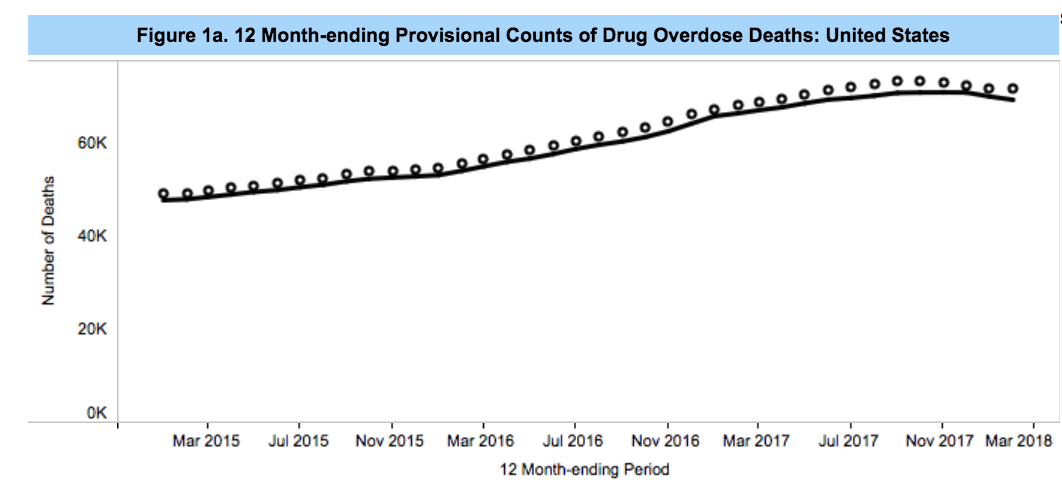
To address the mis-use and diversion of opioids by people, the DEA has proposed an average 10 percent decrease in the 2019 manufacturing quotas for six frequently abused opioids, including five key Class II opioid drugs commonly used by veterinarians. DEA decreased allowable opioid manufacturing quotas by 25 percent in 2017 and 20 percent this year. When supplies of these drugs are limited, manufacturers and distributors give preference to allocating their limited supplies for use in human health, creating shortages for veterinary medical practitioners. For example, in August, Pfizer suspended delivery of injectable opioids to veterinary customers.
According to the survey, these shortages have had the unintended results of creating unnecessary pain, suffering, and death of animals because alternatives are less effective and are more expensive.
Key findings of the survey:
In the past year, from 27% to 73% of veterinary professionals have had difficulty obtaining necessary supplies of five opioids they consider “important to your practice and to your patients’ health” by 50% – 80% of respondents. They include Hydromorphone, Morphine, Fentanyl, Hydrocodone, and Oxymorphone.Shortages of these opioids have caused … The use of less effective, non-narcotic alternatives such as NSAIDS (83%);Increased patient suffering (71%);Use of a local anesthetic (49%);Postponed procedures (26%); andPatient deaths (3%)88% of respondents “rarely” or “never” see the four warning signs published by DEA that a client is potentially abusing opioids. Nevertheless, 63% “have training and/or procedures in place for medical and other staff members to recognize the signs of opioid abuse.”
The survey was conducted in September by Wedgewood Pharmacy, the largest animal-health compounding pharmacy in the U.S. The invitation to participate went to 53,968 veterinary professionals; 1,135 completed the survey. The results (which include hundreds of write-in comments from veterinarians) will be included in formal comments that the company will submit to the DEA regarding the proposed production quota reductions. [DEA will be accepting comments at http://www.regulations.gov until 11:59PM, September 19, 2018. Please reference ‘‘Docket No. DEA–488P’’ on all correspondence, including any attachments.]
Michael Blaire, R.Ph., FIACP, vice president, Government and Regulatory Affairs noted, “Shortages limit therapeutic choices and are especially problematic given the number of species veterinarians treat—from tiny kittens to large dogs, horses, and even elephants—and how different species react to opioids or their alternatives. Shortages demand that veterinarians frequently change medications and pain-management protocols, and this increases the risk of medical errors. While we applaud DEA’s efforts to address the national opioid crisis among humans, we’re asking them to be thoughtful about the impact the actions they take will have on the animal patients owned by 68% of American homes and the millions of animals in zoos, aquaria, stables, shelters, hospitals, research facilities, police and military facilities. We need to work together to address a national crisis in human health while continuing to provide veterinarians with the medicines they need to practice.”
One veterinarian wrote this comment to illustrate how opioid shortages affect his or her patients: “We have an emergency practice, so we see a lot of very painful animals from surgeries, traumas, and severe illness. Most of our patients in acute pain are not candidates for NSAIDS or other treatments like laser and acupuncture, which take longer to work and are not proven effective for severe pain. Not having access to opioids almost makes treatment cruel.”
Wedgewood Pharmacy and recently acquired Diamondback Drugs are licensed by DEA to manufacture controlled substances, which they do exclusively for animal patients. Compounded medications are created and prepared by specially trained pharmacists and pharmacy technicians in nationally accredited, state-regulated facilities, when mass-manufactured drugs are not available or appropriate for a patient. These medications are prescribed and dispensed under orders written by veterinarians. At least one facility has experienced difficulty obtaining the quantities of active pharmaceutical ingredients needed to meet the demands of their veterinary customers, because of purchasing quotas set by DEA.
The sampling of participants in the survey was participant-driven, not random, and therefore measures of statistical significance such as confidence levels and sampling error do not apply to the results of the study. They represent the opinions of the professionals who participated.
About Wedgewood Pharmacy
In its 37 years, Wedgewood Pharmacy has grown from a local community pharmacy to become one of the largest compounding pharmacies in the United States; it is the leading pharmacy in animal health. Wedgewood Pharmacy serves more than 50,000 prescribers and hundreds of thousands of patients throughout the U.S. every year.
George (late) and Lucy Malmberg, both pharmacists, purchased Wedgewood Pharmacy in 1981; the pharmacy was founded in 1980. In June 2016, Chicago-based New Harbor Capital became the majority owner of the company. In July 2018, the company acquired Diamondback Drugs, Scottsdale, Arizona.
Wedgewood Pharmacy is accredited by the Pharmacy Compounding Accreditation Board (PCAB ® ) for compliance with PCAB and other nationally recognized compounding standards. PCAB was formed by eight of the nation’s leading pharmacy associations and is a service of Accreditation Commission for Health Care. As a third-party accreditation organization, PCAB has developed the highest national standards against which providers are measured to demonstrate their ability to effectively and efficiently deliver quality compounded medications to consumers. Wedgewood Pharmacy employs more than 500 people in its state-of-the-art compounding pharmacies in Swedesboro, New Jersey and Scottsdale, Arizona.
View source version on businesswire.com:https://www.businesswire.com/news/home/20180914005480/en/
CONTACT: Wedgewood Pharmacy
Michael Blaire, R.Ph., FIACP
Vice President, Government and Regulatory Affairs
MBlaire@WedgewoodPharmacy.com
Like this:
Like Loading...
Filed under: General Problems | 7 Comments »
 Coca-Cola ‘Closely Watching’ Use of Cannabis in Wellness Drinks
Coca-Cola ‘Closely Watching’ Use of Cannabis in Wellness Drinks