PBM faces suit over alleged ‘refill pill mill’ scheme
https://ncpa.org/newsroom/qam/2022/06/29/pbm-faces-suit-over-alleged-refill-pill-mill-scheme
Express Scripts is facing a lawsuit under the False Claims Act on charges that it delivered pointless prescribed drugs to military personnel, bilking the federal authorities and distributors out of billions of dollars. A whistleblower claims the company’s software was allegedly set up to refill 90-day prescriptions on day 60, which means that
Tricare beneficiary obtained 73 percent more tablets than prescribed over the course of 12 months.
The suit was filed in a California federal courtroom in mid-2019 and unsealed earlier this month. Express Scripts inflated drug prices for payers and patients via its “refill pill mill” that systematically overcharged the Tricare program for treatment from October 2009 to March 2018, the suit alleges. NCPA has spoken out for years against mail-order pharmacy for many reasons, not the least of which is the waste it produces. Here’s a link to our Waste Not, Want Not document showing examples of this needless waste. If you have a photo to add, send it to Michael Rule.
 According to https://en.wikipedia.org/wiki/Express_Scripts One of Express Scripts largest clients is the United States Department of Defense‘s Tricare program. and On March 7, 2018, it was announced that Cigna would buy Express Scripts in a $67 billion deal. The deal closed on December 20, 2018 at $54 billion, allowing Cigna to start offering new Express Scripts products to its corporate health insurance customers in 2019.
According to https://en.wikipedia.org/wiki/Express_Scripts One of Express Scripts largest clients is the United States Department of Defense‘s Tricare program. and On March 7, 2018, it was announced that Cigna would buy Express Scripts in a $67 billion deal. The deal closed on December 20, 2018 at $54 billion, allowing Cigna to start offering new Express Scripts products to its corporate health insurance customers in 2019.
Maybe Cigna’s due diligence in looking into buying Express Scripts, exposed this “little systematic overcharging” of Tricare/Feds caused it to come to a end, because Cigna’s did not have anything to do with the financial liability tail attached to the Express Scripts deal.
Filed under: General Problems



















Another Expresscripts thing is their rule that if you have OPM insurance but get a discount if you buy without insurance at an outside pharmacy (one rx is $300 copay at ES, 10$ cost with coupon at a family pharmacy for 90 pills) they will, if I understand it, not allow you to use ES for that script again. $10 vs $300 is substantial. Why the cost difference and how can they prevent you from getting that savings? It just seems wrong.
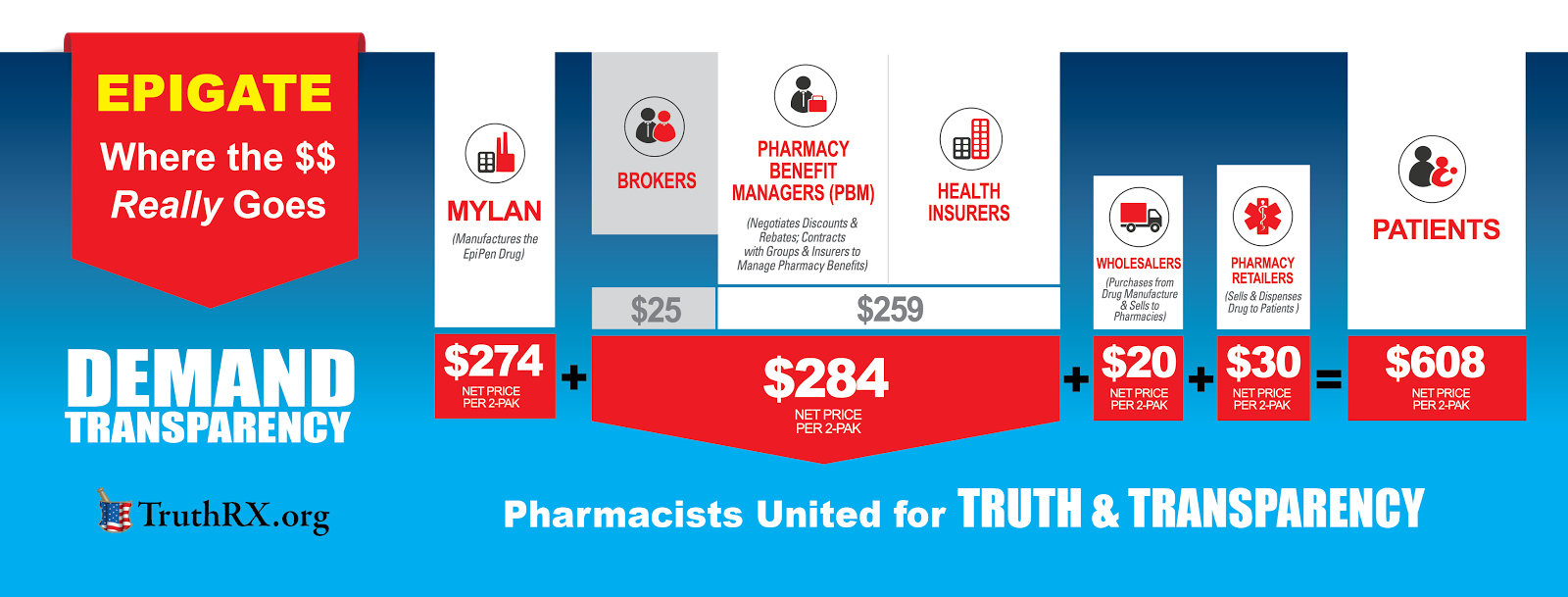
I suspect that is probably “just a rumor”… if they have a website where they state they will pay for a particular med under your policy… and they refuse to pay for it. There is probably a number of entities that the pt can file complaint with… With our Part D, I recently had a Rx filled and Humana Part D … the med is listed on Medicare website that they pay for this generic.. BUT.. they will only pay for the med only produce by a particular pharma.. I have not met my deductible yet, the copay was $56 and my Pharmacist told me that their CASH PRICE for a generic was $36. At one time, these PBM’s had in their contracts with pharmacies that the Pharmacist COULD NOT TELL a pt that -the pharmacy’s cash price WAS LESS – unless the pt asked what the cash price was … Congress actually passed a law to prohibit the PBM industry from having such restrictions in their contracts. It has been stated that the PBM industry will DEMAND a kickback/discount/rebate from the pharma to put their meds on their approved formulary – no prior authorization required to pay for a particular med. It is reported that the collective $$$ the pharma has to pay back to the PBM can be as high as 75% of the AWP ( Average Wholesale Price ) Here is a graphic that demonstrates whose pocket the $$ you pay at the pharmacy register goes into.